Validation of Sterile Filtration: A Comprehensive Overview
Introduction
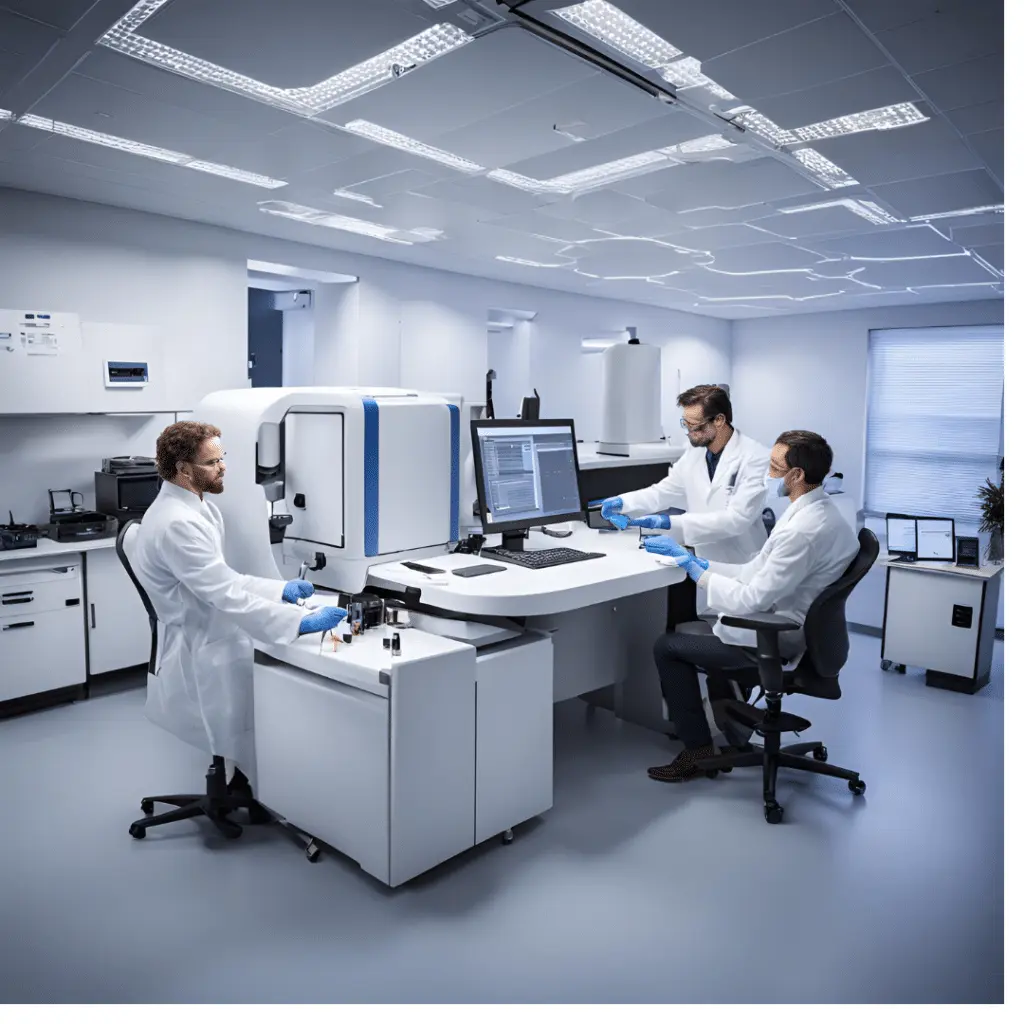
Sterile filtration is a crucial process in pharmaceutical and biopharmaceutical manufacturing. Its main objective is to remove microorganisms from products to ensure sterility without adversely affecting the product’s quality. This process is employed widely for drug products that cannot be heat-sterilized, such as biologics and other temperature-sensitive formulations. Sterile filtration involves passing a fluid through a sterilizing-grade filter, typically rated at 0.2 or 0.22 microns, to remove microorganisms such as bacteria and fungi.
The validation of sterile filtration is essential to ensure that the process consistently produces a sterile filtrate. This article provides a detailed review of the validation process for sterile filtration, including its key principles, protocols, and practical considerations, based on established industry standards and best practices, particularly those outlined in the Parenteral Drug Association’s (PDA) Technical Report No. 26.
Principles of Sterile Filtration
Sterile filtration is designed to ensure that pharmaceutical products, especially those administered parenterally, are free from microbial contamination. The filter membrane’s pore size is the primary determinant of its ability to remove microorganisms, with 0.2 or 0.22-micron filters being standard for sterilizing purposes. These filters are validated to retain a challenge concentration of Brevundimonas diminuta (ATCC 19146), a small, rod-shaped bacterium that can penetrate larger-pore filters. Validation processes focus on demonstrating the filter’s efficacy in real-world conditions, ensuring consistent performance.
Key Elements of Sterile Filtration Validation
-
Filter Integrity Testing
Integrity testing is a critical step in the validation of sterile filters. It ensures that the filter is structurally sound and free of defects that could compromise sterility. Common integrity tests include the bubble point test, forward flow (or diffusive flow) test, and pressure hold test. These tests are designed to detect defects in the filter or its housing that could allow microorganisms to pass through.
– Bubble Point Test: This test measures the pressure at which a liquid is forced out of the filter pores by gas. The pressure at which bubbles first appear indicates the size of the largest pores, ensuring the filter meets the required specification.
– Forward Flow Test: This method assesses the integrity of the filter by measuring the amount of gas passing through the wetted membrane under a constant pressure.
– Pressure Hold Test: This is used for hydrophobic filters and evaluates the ability of the filter to maintain a set pressure over time.
-
Bacterial Challenge Testing
One of the most critical steps in filter validation is the bacterial challenge test, which confirms the filter’s ability to remove microorganisms under specified conditions. The standard bacterium used for validation is B. diminuta, which is challenging to filter due to its small size (0.3 microns). The filter is tested by introducing a high concentration of bacteria (usually 10^7 colony-forming units (CFU) per cm² of filter surface) and demonstrating that none pass through the filter.
-
Filter Compatibility Testing
The materials used in filters must be compatible with the pharmaceutical product and process fluids. This ensures that the filter does not release harmful extractables or interact with the product in a way that affects its purity, potency, or stability. Filter materials must be tested for compatibility with process conditions such as pressure, temperature, and the chemical composition of the fluids.
-
Filter Adsorption Testing
In addition to microbial retention, the filter must be tested for its tendency to adsorb active ingredients, excipients, or other product components. Adsorption can lead to a reduction in the product’s potency, especially in cases involving biologics or protein-based formulations. It is important to demonstrate that the filter does not cause any loss of critical product components.
-
Validation of Process Conditions
Sterile filtration must be validated under the actual processing conditions, including product flow rates, pressure differentials, and processing time. For instance, if a product is filtered over eight hours in production, the validation process must run for at least the same duration. Additionally, the validation must consider the maximum flow rates and differential pressures encountered during normal operations.
Best Practices for Sterile Filtration Validation
-
Defining Critical Parameters
During validation, it is essential to define critical parameters such as flow rate, pressure, temperature, and contact time with the product. These parameters must be controlled and documented to ensure consistent filter performance.
-
Using Worst-Case Scenarios
Validation should be performed under worst-case conditions to ensure robustness. For instance, using the highest anticipated bacterial load or the most challenging fluid to filter ensures that the process will work under all expected production conditions. These worst-case conditions provide a safety margin for real-world production.
-
Redundant Filtration Systems
In some cases, redundant filtration systems are used, especially for high-value or biologically active products. These systems involve using two filters in series to provide an additional safety layer. If both filters are needed to ensure sterility, they must both be validated and tested for integrity after use.
-
Bracketing Approach
The bracketing approach allows manufacturers to validate a range of similar products by challenging only the extreme conditions within a product family. For instance, if different concentrations of the same drug are produced, the highest and lowest concentrations are tested, and the intermediate concentrations are assumed to behave similarly.
Regulatory Guideline
Regulatory agencies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) require that sterile filtration processes be validated according to good manufacturing practices (GMP). Validation documentation must demonstrate that the filtration process consistently produces a sterile product and that the filter is suitable for the intended use.
The PDA’s Technical Report No. 26 is a widely accepted guideline for sterile filtration validation. It outlines the key steps for filter validation, including filter integrity testing, bacterial challenge testing, and compatibility testing. Manufacturers are expected to follow these guidelines and provide thorough documentation of their validation efforts.
Challenges in Sterile Filtration Validation
-
Filter Fouling
Over time, filters may become fouled with particles or microorganisms, reducing flow rates and increasing pressure differentials. Fouling can lead to premature filter failure or the need for frequent filter changes, which can disrupt production. Validation processes must account for the expected level of fouling and include provisions for filter replacement or cleaning.
-
Variability in Bioburden
The bioburden (the number of microorganisms present in the product before filtration) can vary from batch to batch. A higher bioburden increases the likelihood of microbial passage through the filter. Validation must include strategies to control bioburden, such as raw material quality control or pre-filtration steps.
Conclusion
The validation of sterile filtration is a critical step in ensuring the sterility of pharmaceutical products. By following industry guidelines, performing rigorous testing, and documenting the results, manufacturers can ensure that their filtration processes are reliable, robust, and compliant with regulatory requirements. The steps involved in filter integrity testing, bacterial challenge testing, and filter compatibility testing must be carefully executed and validated under real-world conditions to guarantee consistent product safety.
Pharmaceutical manufacturers bear the ultimate responsibility for filter validation, and collaboration with filter manufacturers can help ensure the successful implementation of sterile filtration processes. By adhering to best practices and leveraging worst-case scenarios, manufacturers can build a strong validation framework that ensures the sterility of their products throughout the production lifecycle.